Cornea Transplant in Amritsar
At Dr. Shakeen Eye & Dental Hospital, we specialize in Cornea Transplant in Amritsar, offering advanced and effective treatments to restore vision for patients with damaged, diseased, or scarred corneas. Our expert ophthalmologists use cutting-edge techniques to ensure safe, precise, and successful corneal transplants, helping patients regain clear and healthy vision.
What is a Cornea Transplant?
A cornea transplant (keratoplasty) is a surgical procedure that replaces a damaged or diseased cornea with a healthy donor cornea. The cornea is the clear, dome-shaped front surface of the eye, which plays a crucial role in focusing vision. When it becomes clouded, scarred, or injured, vision becomes blurry or completely lost. A corneal transplant restores clarity and improves eyesight, allowing patients to lead a normal life.
Who Needs a Cornea Transplant?
Keratoconus
A progressive condition that causes the cornea to become thin and cone-shaped.
Corneal Scarring
Caused by infections, injuries, or previous surgeries.
Corneal Dystrophies
Genetic disorders that affect corneal clarity, such as Fuchs’ dystrophy.
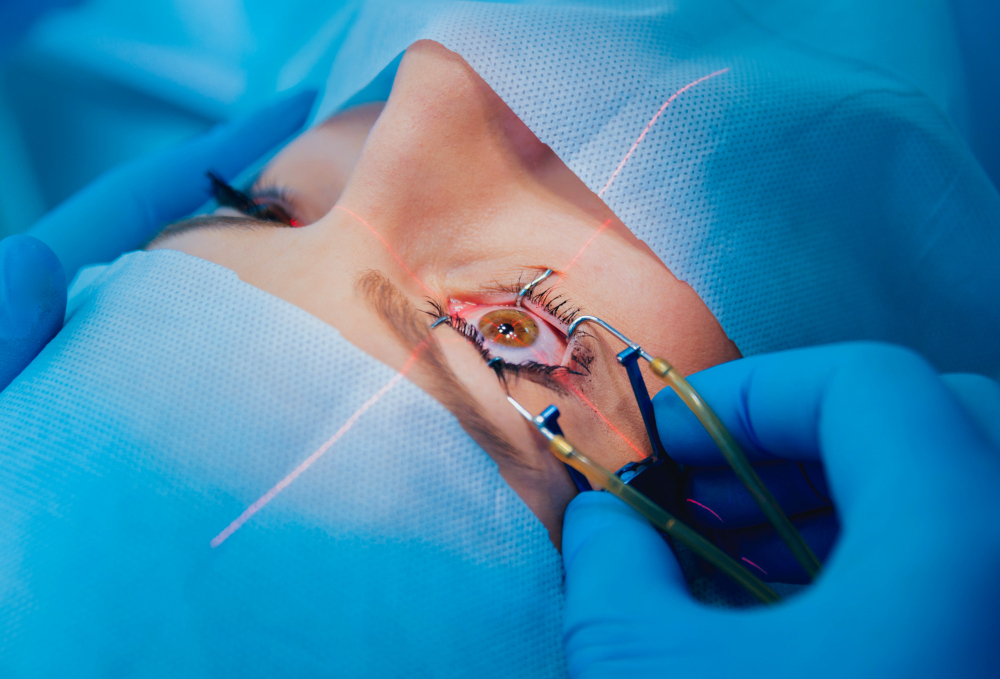
The Cornea Transplant Procedure
- Comprehensive Eye Examination: Our specialists assess your eye health, corneal thickness, and vision condition.
- Donor Cornea Selection: A healthy, high-quality donor cornea is sourced from an eye bank.
- Surgical Procedure: The damaged cornea is removed and replaced with the donor cornea using precise techniques.
Post-Surgery Care & Recovery
- Use prescribed eye drops to prevent infection and rejection.
- Avoid rubbing or putting pressure on the eye.
- Wear protective eyewear for a few weeks.
- Follow up with regular check-ups to monitor healing.

Regain Clear Vision with Cornea Transplant in Amritsar!
If you or a loved one is struggling with vision loss due to corneal disease, don’t wait! Book a consultation today at Dr. Shakeen Eye & Dental Hospital and take the first step toward restoring your sight.
